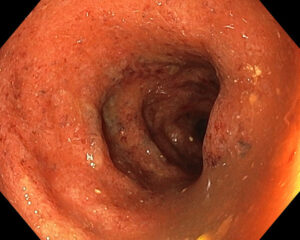
Ulcerative Colitis and Crohn's disease
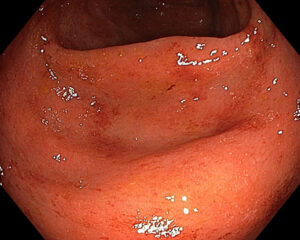
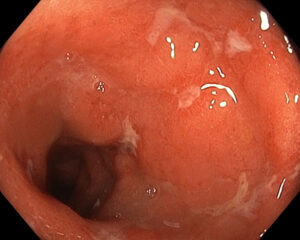
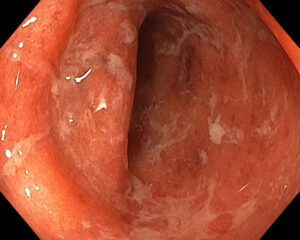
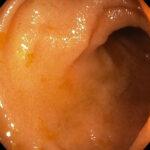
Inflammatory bowel disease refers to a two main diseases, Ulcerative colitis (UC) and Crohn’s disease that cause ulceration and inflammation of the bowel.
Common symptoms include diarrhoea, rectal bleeding, passing mucous, abdominal pain, bloating and sometimes weight loss.
Despite a lot of research the exact cause of these diseases remains unknown. In both cases damage occurs to the bowel due to inflammation that is driven by a dysfunctional and overactive immune system. Treatments are therefore targeted at reducing inflammation and dampening down the immune system.